Pelvic pain and urinary frequency can be disabling. What is Interstitial Cystitis? How is Interstitial Cystitis diagnosed? What causes Interstitial Cystitis? What are Interstitial Cystitis natural treatment options? Let’s dig in.
What is Interstitial Cystitis?
Interstitial Cystitis also referred to as painful bladder syndrome or hypersensitive bladder, is a potentially devastating chronic bladder condition that consists of multiple symptoms which include:
- Recurring pelvic pain, pressure or discomfort in the bladder and pelvic region
- Urinary frequency (needing to go often)
- Urinary urgency (feeling a strong need to go)
Interstitial Cystitis (IC) disproportionately affects women more than men. Awareness of the condition and its impact on both physical and psychological well being has brought increased attention and study to Interstitial Cystitis. Unfortunately, as is the case when multiple experts come together there are differing opinion and thoughts. Unfortunately, there is no consensus on the definition of Interstitial Cystitis (1). Different academic organizations have different criteria and definitions for the diagnosis as highlighted below:
The International Continence Society (ICS)
Suprapubic pain related to bladder filling, accompanied by other symptoms such as increased daytime and night time frequency, in the absence of proven urinary infection or other pathology (2).
The European Society for the Study of Interstitial Cystitis
Chronic pelvic pain, pressure, or discomfort perceived to be related to the urinary bladder accompanied by at least one other urinary symptom such as a persistent urge to void or urinary frequency (3).
The Society for Urodynamics, Female Pelvic Medicine & Urogenital Reconstruction (SUFU)
An unpleasant sensation (pain, pressure, discomfort) perceived to be related to the urinary bladder, associated with lower urinary tract symptoms of more than six weeks duration, in the absence of infection or other identifiable causes (4).
To complicate matters more there are different sub-types of interstitial cystitis based upon the presence of Hunner lesions found during a visual inspection of the bladder wall. Hunner lesions are reddened mucosal areas with small vessels radiating toward a central scar (5).
How Is Interstitial Cystitis Diagnosed?
Interstitial Cystitis can be difficult to diagnose due to varying diagnostic criteria as illustrated above. It is further complicated by the fact that its symptoms overlap with other conditions such as urinary tract infection, overactive bladder, and endometriosis. Often times these other conditions must be worked up and excluded prior to the diagnosis of IC leading to a delay in treatment.
What Is the Cause of Interstitial Cystitis?
The precise cause of interstitial cystitis is unknown. One proposed theory is the activation of specific receptors in the bladder muscle wall by inflammatory chemicals which in turn trigger pain, urinary frequency, and swelling (6). Interstitial cystitis natural treatments accordingly focus on the reduction of inflammation.
Treatment Options
Multiple treatment options exist which include
- Elimination diets (7)
- Oral medications
- Bladder medications
- Pelvic Floor Physical Therapy (8)
- Botox injections
- Trigger point injections
- Pudendal nerve blocks (9)
- Stimulation of sacral nerve roots with an indwelling neurostimulation device.
Interstitial Cystitis Natural Treatment
Interstitial cystitis natural treatment options include melatonin which protects the bladder lining and quercetin which is an antioxidant. Using your body’s own healing capacity is another viable natural treatment option. Specifically, a patient’s own platelets can be injected into the low back nerves.
How Can the Low Back and the Bladder Be Connected?
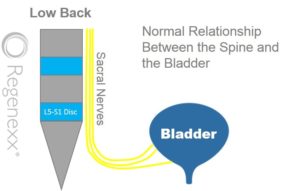
The illustration to the left shows the sacral nerves exiting the low back near the lowest disc level, L5/S1. The sacral nerves then travel to the bladder and act as a conduit for bladder sensation. In the absence of any irritation or pressure on the nerves, the sacral nerves allow transmission of the normal bladder sensation from the bladder to the brain.
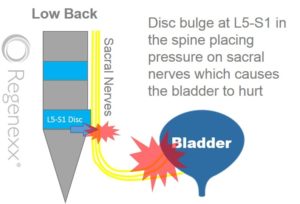
The illustration to the right demonstrates what happens when an L5/S1 disc protrusion, herniation or slippage occurs. This can cause pressure and irritation of the sacral nerves. The irritated sacral nerves, in turn, can cause pain and spasm in the bladder. They can also make a patient believe that the bladder is full when it’s not. All this can occur because the electrical impulses that represent bladder sensation get disrupted by irritated sacral nerves.
The Centeno-Schultz Clinic has extensive experience in the treatment of low back and nerve injuries. We have also successfully treated patients with Interstitial Cystitis that had sacral nerve irritation due to disc protrusions or herniations. Steroids injections are toxic with significant side effects and therefore avoided. A novel approach is utilized where a patient’s own concentrated platelets are injected. At the Centeno-Schultz Clinic, a special PRP is used called Platelet Lysate which is rich in growth factors that can increase blood flow and decrease inflammation. To learn more about Platelet Lysate and the harmful side effects of epidural steroids please click on the video below.
In Conclusion
Interstitial Cystitis, also known as painful bladder syndrome or hypersensitive bladder, is a chronic symptom complex of the bladder characterized by lower pelvic pain, urinary frequency, and urgency. Because of differing opinions on criteria and definitions, there is no consensus on the definition of interstitial cystitis. The diagnosis can be difficult due to overlap with other conditions. The exact cause of interstitial cystitis is unknown. Multiple treatment options exist. Interstitial cystitis natural treatments include supplements. An often neglected cause of Interstitial Cystitis is irritation of the sacral nerves. A novel treatment exists with the injection of irritated sacral nerves with a patient’s own platelets.
1.Han E, Nguyen L, Sirls L, Peters K. Current best practice management of interstitial cystitis/bladder pain syndrome. Ther Adv Urol. 2018;10(7):197–211. Published 2018 Mar 19. doi:10.1177/1756287218761574
2.Abrams, P, Cardozo, L, Fall, M. The standardisation of terminology of lower urinary tract function: report from the standardisation sub-committee of the international continence society. Neurourol Urodyn 2002; 21: 167–178.DOI: 10.1002/nau.10052.
3.van de Merwe, JP, Nordling, J, Bouchelouche, P. Diagnostic criteria, classification, and nomenclature for painful bladder syndrome/interstitial cystitis: an ESSIC proposal. Eur Urol 2008; 53: 60–67.DOI: 10.1016/j.eururo.2007.09.019.
4.Hanno, PM, Erickson, D, Moldwin, R. Diagnosis and treatment of interstitial cystitis/bladder pain syndrome: AUA guideline amendment. J Urol 2015; 193: 1545–1553.DOI: 10.1016/j.juro.2015.01.086
5.Fall, M, Logadottir, Y, Peeker, R. Interstitial cystitis is bladder pain syndrome with Hunner’s lesion. Int J Urol 2014; 21(Suppl. 1): 79–82.DOI: 10.1111/iju.12325.
6.Wajih Ullah M, Lakhani S, Sham S, Rehman A, Siddiq W, Siddiqui T. Painful Bladder Syndrome/Interstitial Cystitis Successful Treatment with Montelukast: A Case Report and Literature Review. Cureus. 2018;10(6):e2876. Published 2018 Jun 25. doi:10.7759/cureus.2876
7. Oh-Oka, H . Clinical efficacy of 1-year intensive systematic dietary manipulation as complementary and alternative medicine therapies on female patients with interstitial cystitis/bladder pain syndrome. Urology 2017; 106: 50–54.DOI: 10.1016/j.urology.2017.02.053.
8. Weiss, JM . Pelvic floor myofascial trigger points: manual therapy for interstitial cystitis and the urgency-frequency syndrome. J Urol 2001; 166: 2226–2231.DOI: 10.1016/s0022-5347(05)65539-5
9.Labat, JJ, Riant, T, Robert, R. Diagnostic criteria for pudendal neuralgia by pudendal nerve entrapment (Nantes criteria). Neurourol Urodyn 2008; 27: 306–310.DOI: 10.1002/nau.20505.