Lumbar disc bulges are a common cause of lower back and leg pain, impacting a significant number of individuals worldwide. These spinal discs, situated between the vertebrae, act as shock absorbers and facilitate spinal movement. However, when a disc bulges, it exerts pressure on nearby nerves, particularly those extending into the legs.
This compression can result in radiating pain, tingling, or numbness along the affected nerve pathway. Understanding how lumbar disc bulges contribute to leg discomfort is crucial for individuals seeking relief and effective management of their lower back and leg pain.
What Is a Bulging Disc?
A bulging disc refers to a condition affecting the spine, specifically the intervertebral discs that act as cushions between the vertebrae. These discs have a tough outer layer (annulus fibrosus) and a soft gel-like inner core (nucleus pulposus). In the case of a bulging disc, the outer layer weakens or protrudes beyond its usual boundaries, often due to age-related wear and tear, trauma, or repetitive strain.
Bulging Disc Vs. Herniated Disc
It’s important to differentiate between a bulging disc and a herniated disc. While both involve issues with the disc’s structural integrity, a bulging disc occurs when the outer layer protrudes more generally and can be symmetric or slightly asymmetric.
On the other hand, a herniated disc involves a more severe injury of the annular fibers, with the inner core pushing through a tear in the outer layer. This key distinction helps in understanding the varied symptoms and potential treatment approaches for each condition.
Contained Disc Vs. Non-Contained Disc Disorders
Contained and non-contained disc disorders refer to different conditions affecting the intervertebral discs in the spine, specifically in the back or neck. These disorders are commonly associated with disc herniation and play a crucial role in understanding the severity and potential treatment options.
In a contained disc disorder, the integrity of the intervertebral disc’s outer layer is maintained. This outer layer is known as the annulus fibrosis. It prevents the gel-like inner core, known as the nucleus pulposus, from extrusion.
The disc may protrude, causing pressure on nearby nerves, but the outer layer remains intact. Symptoms can include localized or radiating pain, tingling, and muscle weakness. Conservative treatments such as physical therapy, medications, and lifestyle modifications are often considered before more invasive options.
A non-contained disc disorder, on the other hand, occurs when the outer layer of the disc is compromised, leading to the leakage or herniation of the inner core into the surrounding area. This condition can be more severe than a contained disorder, as the material from the disc can irritate or compress nearby nerves, resulting in more intense and widespread symptoms.
Treatment options for non-contained disc disorders may involve a combination of conservative measures like physical therapy and medications, as well as more aggressive interventions such as epidural injections or surgical procedures, depending on the severity and impact on the individual’s quality of life.
Three Areas Where Bulging Discs Can Occur
The spine is divided into three main regions: cervical (neck), thoracic (mid-back), and lumbar (lower back). Disc bulges can occur in any of these areas, each potentially giving rise to distinct symptoms and referred pain.
Cervical
In the cervical spine, a bulging disc may lead to referred pain, such as numbness or tingling in the arms. This discomfort often radiates down one or both arms, affecting mobility and sensation.
Thoracic
When a bulging disc occurs in the thoracic spine, it may result in referred pain in areas such as the chest, abdomen, or even the legs. This can manifest as pain, numbness, or tingling sensations in the upper or lower extremities, sometimes even mimicking conditions like sciatica.
Lumbar
The focus of this article is on lumbar disc bulges, which predominantly affect the lower back. When a disc bulges in the lumbar spine, it commonly causes referred pain down the legs, known as sciatica. Symptoms may include sharp shooting pain, numbness, or weakness, and the discomfort often follows the path of the affected nerve, extending from the lower back into the buttocks and down one or both legs.
Lumbar Disc Bulges and Leg Pain
Leg pain is a prevalent symptom of a bulging disc in the lumbar spine due to the anatomy of the spinal nerves and the compression or irritation caused by the bulge.
Here are key reasons why leg pain often occurs:
- Nerve compression: The spinal nerves that control sensation and movement in the lower body originate from the lumbar spine. A bulging disc can put pressure on these nerves, leading to compression or irritation.
- Sciatic nerve involvement: The largest and longest nerve in the body, the sciatic nerve, runs down the back of each leg. When a lumbar disc bulges, it can impinge on the roots of the sciatic nerve, causing pain that radiates along its pathway.
- Radicular pain: The pain experienced is often radicular, meaning it follows the path of the affected nerve. This can result in sharp, shooting pain traveling from the lower back into the buttocks and down the leg.
- Inflammatory response: The disc material that protrudes from the bulging disc can trigger an inflammatory response, exacerbating nerve irritation and contributing to pain in the legs.
- Muscle weakness and numbness: Nerve compression can lead to muscle weakness and numbness in the affected leg. This may impact balance, coordination, and the ability to perform daily activities.
- Sensory changes: Individuals with a lumbar disc bulge may experience sensory changes, such as tingling or a “pins and needles” sensation, along the course of the affected nerve.
- Aggravation with movement: Certain movements, such as bending, lifting, or sitting for prolonged periods can exacerbate the compression on the nerves, intensifying leg pain.
Other Symptoms You Should Look Out For
The severity and specific location of the disc bulge play a pivotal role in determining the variety and intensity of symptoms experienced by individuals. Below are some symptoms you should watch out for.
Back Muscle Spasms
The severity and location of a bulging disc can contribute to back muscle spasms. As the disc bulge affects the stability of the spine and surrounding structures, the body may respond with involuntary muscle contractions. These spasms can lead to additional discomfort, limiting mobility and exacerbating pain in the affected region.
Difficulty Walking
The impact of a bulging disc on nerve function can result in difficulty walking. This symptom may manifest as a combination of muscle weakness, numbness, and pain, affecting the ability to maintain a normal gait. Individuals may experience instability and find it challenging to walk for extended periods or cover certain distances.
Sciatica
While leg pain is a common manifestation of a lumbar disc bulge, it often presents as sciatica. Sciatica refers to the radiating pain that follows the path of the sciatic nerve, running down the buttocks and into one or both legs. This can lead to sharp, shooting pain, tingling, and numbness, with the severity dependent on the degree of nerve compression.
Reduced Coordination
Bulging discs can impact the nerves responsible for coordinating muscle movements. As a result, individuals may experience reduced coordination, affecting their ability to perform precise movements and maintain balance. This symptom can contribute to a higher risk of falls and diminished overall functional capacity.
Therapies for Disc Bulges in Lumbar Spine
Common therapies for lumbar disc bulges include:
- Physical therapy: Physical therapy is a key component in the conservative management of disc bulges in the lumbar spine. A skilled physical therapist designs a personalized exercise program to address specific issues related to the bulging disc. These exercises typically focus on spinal posture and alignment, better activation of the core muscles, glut muscle activation, improving hip flexibility, and enhancing overall spinal stability. Additionally, therapists may employ manual techniques, such as massage, stretching, and nerve flossing to alleviate muscle tension, nerve tension, and promote proper alignment. The goal of physical therapy is to reduce pain, improve function, and equip individuals with long-term strategies for maintaining a healthy spine.
- Lumbar traction: Lumbar traction is a therapeutic technique aimed at decompressing the spine and relieving pressure on the affected discs. During lumbar traction, individuals lie on a traction table, and a controlled pulling force is applied to the lumbar spine. This gentle stretching helps create space between vertebrae, reducing compression on the discs and promoting the influx of nutrients and oxygen to the affected area. Lumbar traction is often used to alleviate pain associated with disc bulges and improve overall spinal mobility.
- Inversion table therapy: Inversion table therapy involves inverting the body to an upside-down position, with the head lower than the feet. This gravitational force assists in stretching and decompressing the spine, potentially reducing the pressure on bulging discs. Inversion tables are designed to allow individuals to control the degree of inversion, making it a customizable therapy option. While some people report relief from symptoms such as back pain and sciatica with inversion therapy, it’s essential to consult with a healthcare professional before incorporating it into a treatment plan, especially for those with certain medical conditions.
- Lumbar epidural steroid injections: Lumbar epidural steroid injections may help pain by reducing inflammation around the irritated nerve. These should always be performed under X-ray to ensure accurate placement of the medication. The epidural space is the area immediately outside the spinal cord and adjacent to the lumbar disc.
If a lumbar epidural steroid is performed without an X-ray there is no guarantee that the medication will get into the epidural space, let alone on the irritated nerve root and disc.
The goal of therapy is to decrease the disc bulge and its compressive effect on the nerve root. If nerve compression is left untreated, it can cause permanent leg pain and weakness.
How We Approach the Treatment for Lumbar Bulging Disc
At the Centeno-Schultz Clinic, we focus on regenerative treatment options for spinal disk bulges. If conservative therapy or lumbar epidural steroid injections cannot provide sustained pain relief, patients now have the option of using their own platelet rich plasma (PRP) to repair their lumbar disc bulges using the Regenexx procedure.
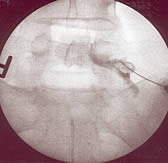
Regenexx is a simple needle-in-needle-out procedure that allows patients to avoid the risks of surgery and anesthesia and repair disc bulges. Using fluoroscopic guidance (real-time X-ray imaging), the regenerative material is precisely injected into the affected area, targeting the lumbar disc bulge. Injection of contrast before the injection of medication ensures accurate placement. The X-ray on the right shows contrast flowing along the right L5 nerve root with extension into the epidural space.
This accuracy helps ensure that the PRP is delivered to the specific location that requires healing. The PRP is rich in growth factors and has the potential to stimulate the body’s natural healing processes.
Additionally, we perform what we call a Perc Functional Spinal Unit procedure (Regenexx Degenerative Disc Disease (DDD) Procedure for Disc Bulges (youtube.com)). With this procedure we address ALL of the components of the spine that are affected when you have a disk bulge. What’s often not explained to patients is that, when one has a disk bulge, the spinal level where that occurs becomes unstable. This instability loosens the ligaments and can cause more pressure on the nerves, disks, and facet joints. Patients also typically have atrophied multifidus muscles as well. So instead of merely injecting epidurally, we need to often treat the supraspinous, interspinous, and intertransverse ligaments, facet joints, and multifidus muscles. This functional spinal unit approach addresses the underlying causes and consequences of disk bulges providing better and longer term relief. This can also help to reduce the need for surgery. Mostly, PRP is used to treat lumbar disk bulges but sometimes bone marrow concentrate containing stem cells are required.
Alleviate the Pain at the Root of the Cause
If you find yourself grappling with persistent symptoms such as lower back pain, radiating leg discomfort, or mobility issues, it is crucial to address the root cause of your distress. Seeking the expertise of a physician is paramount in navigating the complexities of conditions like lumbar disc bulges.
As outlined in the discussion above, a range of therapeutic interventions, from physical therapy to innovative regenerative procedures, offers hope in alleviating pain and improving overall spinal health.
Don’t let persistent pain compromise your quality of life – take the initiative to consult with a physician who can guide you through the most appropriate and personalized course of action. By addressing the root of the cause, you pave the way for a more comfortable and active future.
Regenexx Back Form